The Thoracolumbar Fascia: Its Resilience and Role in Low Back Pain
Introduction
Low back pain (LBP) is one of the most prevalent musculoskeletal conditions, affecting up to 80% of adults globally and accounting for significant healthcare costs and lost productivity (Maher et al., 2017). While the role of muscles, discs, and vertebrae in LBP is well-documented, the thoracolumbar fascia (TLF) has emerged as a key player in spinal health and dysfunction.
The TLF serves as a vital biomechanical interface, connecting muscles to the spine and distributing mechanical loads. This article reviews the anatomy and function of the TLF, its resilience under mechanical stress, and its protective mechanisms against LBP. Evidence supporting its role in spinal stability and therapeutic approaches for maintaining TLF health is also discussed.
Anatomy of the Thoracolumbar Fascia
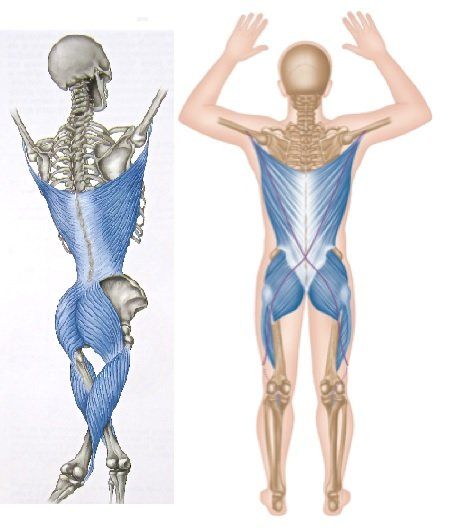
The thoracolumbar fascia is a complex structure composed of three layers—anterior, middle, and posterior—encasing the back's deep musculature, including the erector spinae, multifidus, and quadratus lumborum.
Key Structural Features
- Collagen and Elastin Matrix: Primarily composed of type I collagen, the TLF provides tensile strength and elasticity to withstand mechanical forces (Stecco et al., 2018).
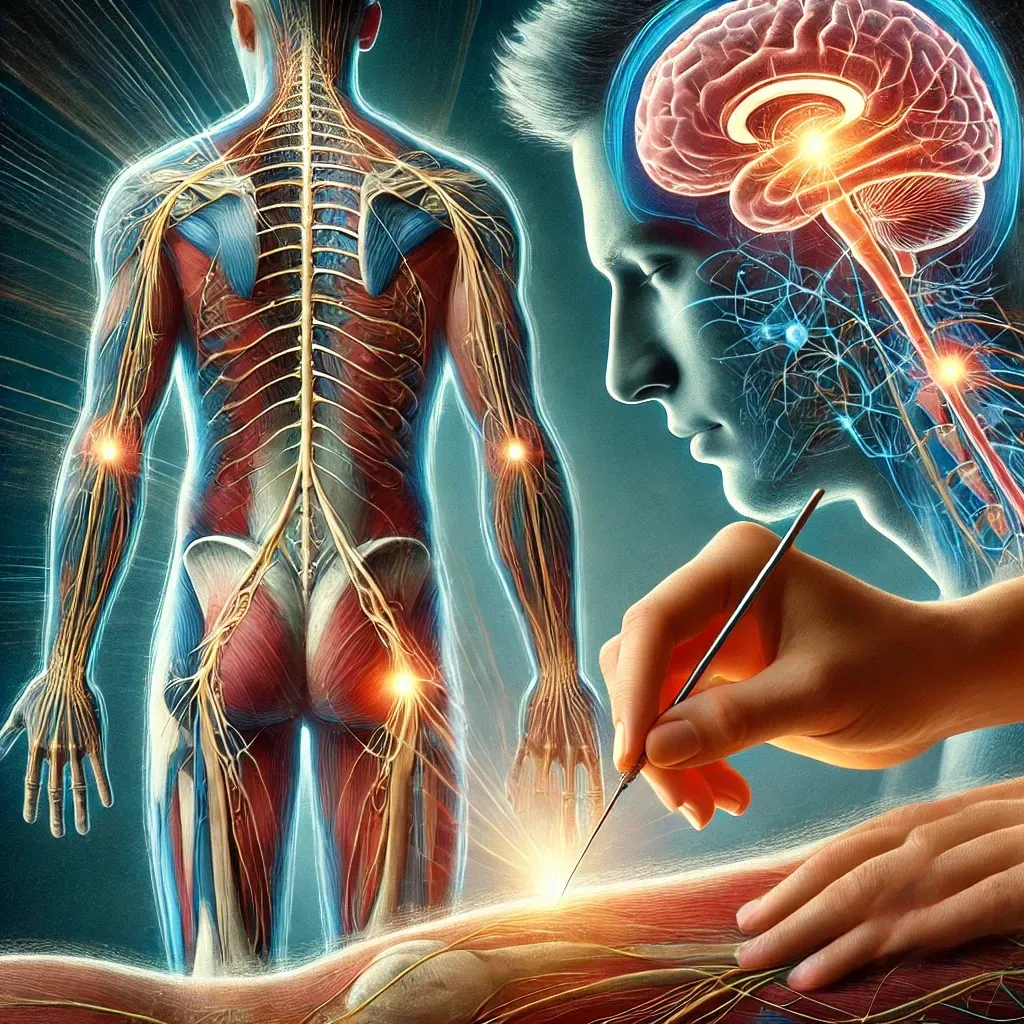
- Neurological Innervation: Richly innervated by sensory and nociceptive fibers, the TLF plays a significant role in proprioception and pain signaling (Fascia Research Congress, 2015).
- Mechanical Role: Acting as a passive stabilizer, it spans the thoracic to lumbar regions, transmitting forces between the upper and lower body.
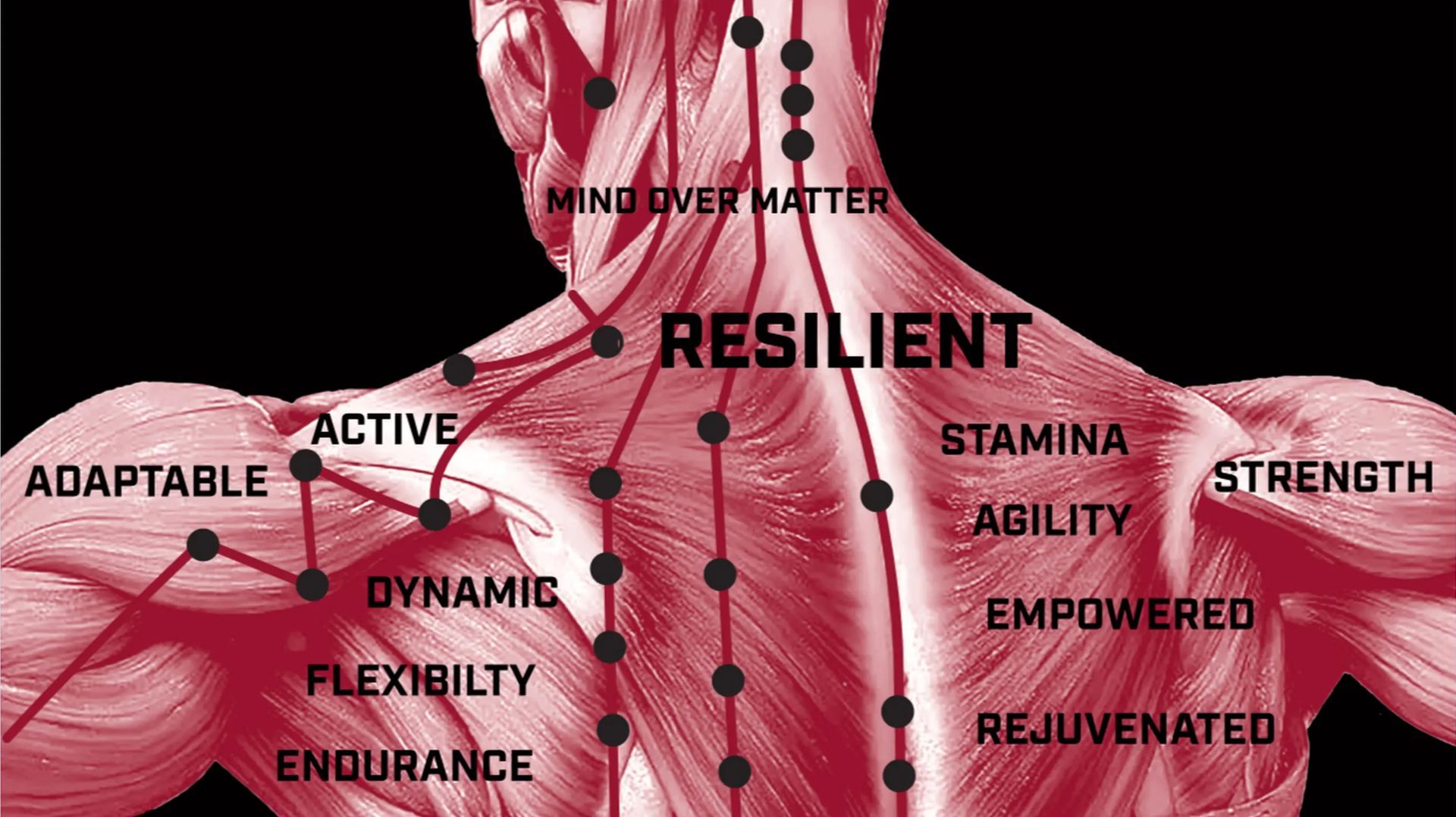
Biomechanics and Resilience of the TLF
The thoracolumbar fascia exhibits remarkable resilience under mechanical stress, contributing to spinal stability and load distribution.
Biomechanical Functions
- Force Transmission: The TLF transmits forces between the upper and lower extremities, reducing localized strain on the lumbar vertebrae (Vleeming et al., 1995).
- Load Sharing: Its multilayered structure allows even distribution of mechanical loads across the thoracolumbar region, preventing overloading of individual structures (Yahia et al., 1992).
- Elastic Properties: The elastin fibers enable the TLF to stretch and recoil during dynamic movements, enhancing its adaptability (Schleip et al., 2019).
Protective Mechanisms
- Shear Force Reduction: By tensioning during movement, the TLF reduces shearing forces on the lumbar spine.
- Core Stability: The TLF enhances the stiffness of the lumbar region, aiding in spinal stabilization during lifting or twisting activities (Hodges & Richardson, 1996).
- Proprioception: Its innervation provides feedback for coordinated muscle activation, ensuring proper spinal alignment.
The TLF and Low Back Pain
Despite its resilience, the thoracolumbar fascia is not immune to dysfunction, which can contribute to the development and persistence of low back pain.
Dysfunction in the TLF
- Fibrosis: Chronic inflammation or repetitive stress can lead to fibrosis, reducing the TLF's elasticity and adaptability (Langevin et al., 2011).
- Adhesions: Scar tissue formation disrupts the sliding properties of the fascia, increasing mechanical strain on surrounding structures (Stecco et al., 2018).
- Pain Sensitization: Overactivation of nociceptive fibers in the TLF can result in chronic pain syndromes (Fascia Research Congress, 2015).
Evidence Linking TLF and LBP
- Imaging Studies: Ultrasound and elastography studies show reduced thickness and impaired sliding of the TLF in LBP patients (Langevin et al., 2011).
- Histological Analysis: Altered collagen structure and increased fibrosis are common findings in the TLF of individuals with chronic LBP (Stecco et al., 2018).
- Therapeutic Studies: Manual therapies targeting the TLF, such as myofascial release, have demonstrated reductions in LBP (Chaudhary et al., 2016).
Evidence-Based Interventions for TLF Health
Maintaining the health of the thoracolumbar fascia is critical for preventing and managing LBP.
- Exercise Therapy
- Core Strengthening: Exercises targeting the multifidus and transverse abdominis improve TLF tension and spinal stability.
- Mobility Drills: Dynamic stretching enhances the TLF's elasticity and adaptability.
- Manual Therapy
- Myofascial Release: Reduces adhesions and restores the TLF's sliding properties.
- Instrument-Assisted Techniques: Promotes collagen remodeling and increases fascial mobility.
- Ergonomics
- Proper posture, lifting techniques, and ergonomic workspace design minimize strain on the TLF.
- Lifestyle Modifications
- Staying hydrated, maintaining a healthy weight, and avoiding prolonged static postures are essential for fascial health.
Emerging Research and Innovations
- Advanced Imaging: MRI and elastography are being explored to assess the TLF's mechanical properties in real-time.
- Regenerative Medicine: Therapies targeting fibrosis and promoting collagen remodeling are under investigation.
- Pain Modulation: Research into the role of the TLF in central sensitization is shedding light on chronic pain mechanisms.
Conclusion
The thoracolumbar fascia plays a vital role in mechanical stability, proprioception, and pain modulation in the lumbar region. Its resilience protects against LBP, but dysfunction within the TLF can lead to chronic pain syndromes. Maintaining TLF health through exercise, manual therapy, and ergonomic practices is essential for spinal health. Future research into advanced imaging and regenerative therapies holds promise for improving outcomes in LBP management.
FAQs
- What is the function of the thoracolumbar fascia?
The TLF stabilizes the lumbar spine, distributes mechanical loads, and provides proprioceptive feedback for coordinated movements. - How does thoracolumbar fascia dysfunction cause pain?
Fibrosis, adhesions, and sensitization within the TLF can disrupt its biomechanics and amplify pain signals, contributing to low back pain. - What exercises benefit the TLF?
Core strengthening exercises, such as planks and bird-dogs, and stretching routines targeting the lower back can enhance the TLF's functionality. - What therapies target the TLF?
Myofascial release and instrument-assisted mobilization are effective for relieving TLF dysfunction and reducing pain. - Can imaging detect TLF problems?
Yes, elastography can reveal structural and functional abnormalities in the TLF, aiding in diagnosis and treatment planning.
References
- Chaudhary, D., Sharma, R., & Agarwal, S. (2016). Myofascial release: An effective approach for managing low back pain. Journal of Physical Therapy Science, 28(3), 771–776. https://doi.org/10.1589/jpts.28.771
- Fascia Research Congress. (2015). Sensory and nociceptive innervation of fascia: Implications for low back pain. Journal of Bodywork and Movement Therapies, 19(4), 567–573. https://doi.org/10.1016/j.jbmt.2015.01.005
- Hodges, P. W., & Richardson, C. A. (1996). Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine, 21(22), 2640–2650. https://doi.org/10.1097/00007632-199611150-00014
- Langevin, H. M., Fox, J. R., Koptiuch, C., Badger, G. J., Greenan-Naumann, A. C., Bouffard, N. A., … Henry, S. M. (2011). Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskeletal Disorders, 12(1), 203. https://doi.org/10.1186/1471-2474-12-203
- Maher, C., Underwood, M., & Buchbinder, R. (2017). Non-specific low back pain. The Lancet, 389(10070), 736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
- McGill, S. M., Grenier, S., Kavcic, N., & Cholewicki, J. (2003). Coordination of muscle activity to assure stability of the lumbar spine. Journal of Electromyography and Kinesiology, 13(4), 353–359. https://doi.org/10.1016/S1050-6411(03)00043-9
- Schleip, R., Stecco, C., & Yucesoy, C. A. (2019). Fascial tissue research in sports medicine: From molecules to tissue adaptation, injury, and diagnostics. International Journal of Sports Medicine, 40(9), 588–599. https://doi.org/10.1055/a-0923-4479
- Stecco, C., Macchi, V., Porzionato, A., Tiengo, C., Parenti, A., & De Caro, R. (2018). The anatomical and functional relation between fascia and muscle. Surgical and Radiologic Anatomy, 40(3), 291–298. https://doi.org/10.1007/s00276-018-1961-0
- Vleeming, A., Stoeckart, R., Volkers, A. C. W., & Snijders, C. J. (1995). Relation between form and function in the sacroiliac joint, part 1: Biomechanical aspects. Spine, 15(8), 1302–1310. https://doi.org/10.1097/00007632-199508001-00015
- Yahia, L. H., Newman, N., & Parnianpour, M. (1992). Mechanical properties and function of the human thoracolumbar fascia. Journal of Biomedical Engineering, 14(5), 379–385. https://doi.org/10.1016/0141-5425(92)90008-Z