Why Cash-Based Practices Deliver Superior Quality Care
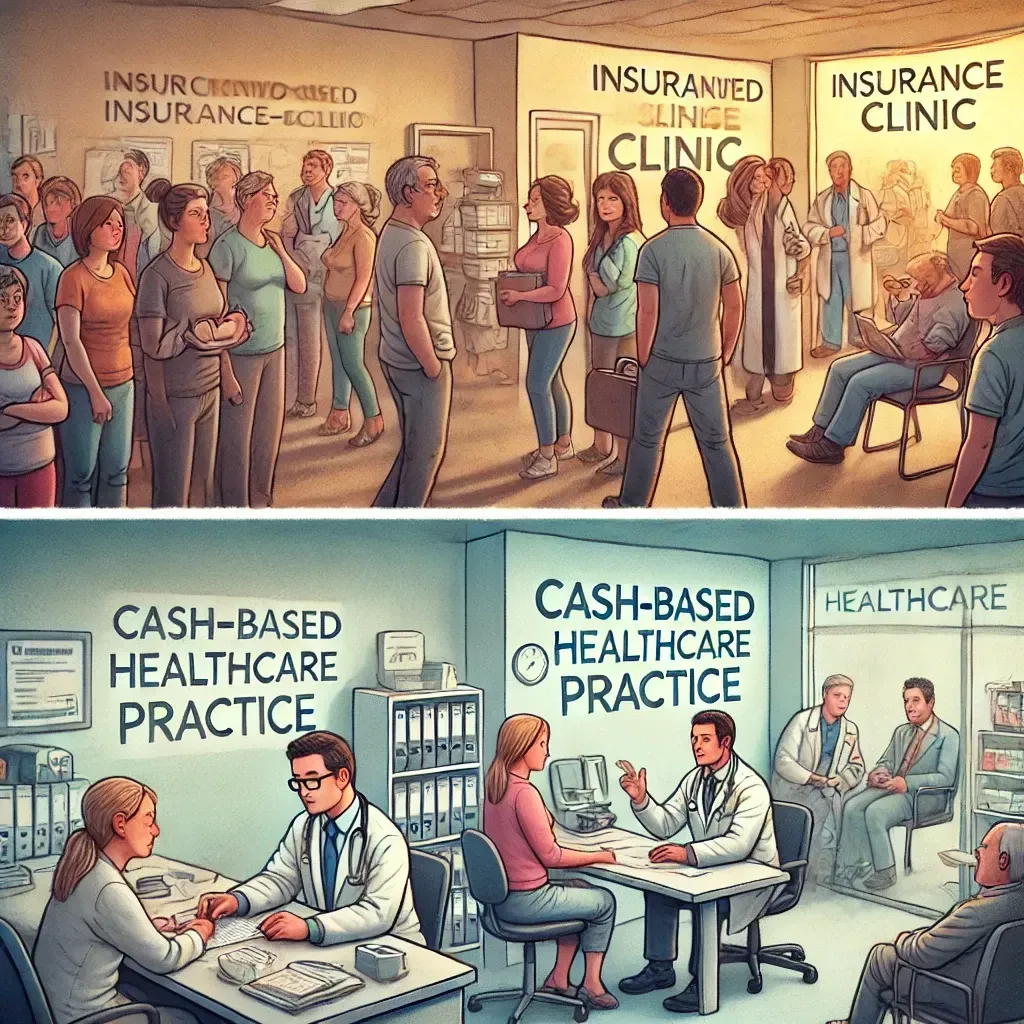
In today’s healthcare system, the insurance-based model dominates. Many patients find themselves stuck within the limitations of insurance coverage, navigating through administrative red tape and rushed appointments. Meanwhile, a growing number of healthcare providers are choosing to operate outside of this system, opting for cash-based practices where they have greater control over their care and the time they spend with patients. This shift is leading to higher quality care and better patient outcomes, and here’s why.
The Drawbacks of Insurance-Based Healthcare
1. Time Constraints and High Patient Volume
Under an insurance-based model, providers are often incentivized to see as many patients as possible in a day. The volume-driven nature of this system limits the time physicians, physical therapists, acupuncturists, and other providers can spend with each patient. Recent studies show that shorter visits, often under 20 minutes, are associated with reduced patient satisfaction and worse health outcomes (Ray et al., 2019).
The result? A transactional experience where both patient and provider are focused on efficiency over depth. Patients can leave feeling rushed, unheard, and without the thorough care they deserve. Providers also face burnout, unable to practice medicine in the thoughtful, patient-centric manner they envisioned when entering the field.
2. Insurance Dictating Care
Insurance companies hold significant power in deciding what treatments or procedures are covered, often leading to restrictions that affect patient outcomes. These decisions are driven by cost containment rather than patient health, resulting in limited access to necessary services. For example, recent research found that many insurance plans restrict access to rehabilitative therapies, leading to suboptimal recovery (Thomson et al., 2021).
Additionally, alternative treatments like acupuncture, which have been shown to be effective in managing chronic pain, are often not covered by insurance, despite their evidence-based benefits (Vickers et al., 2018).
3. Excessive Administrative Burdens
Insurance paperwork, claim submissions, and billing inquiries consume valuable time and resources that could otherwise be dedicated to patient care. Providers are often forced to hire additional staff just to handle administrative tasks, driving up operational costs and reducing the focus on quality care. Recent estimates suggest that administrative costs in the U.S. healthcare system account for about 34% of total healthcare spending, significantly impacting both provider efficiency and patient satisfaction (Shen et al., 2020).
For patients, denied claims, out-of-network fees, and complex billing processes contribute to increased stress and poorer care experiences.
How Cash-Based Practices Offer Better Care
1. Personalized and Unrushed Care
In a cash-based model, providers aren’t restricted by insurance reimbursement structures, allowing them to spend more time with each patient. This results in more personalized, in-depth care. A recent study highlighted that longer visit times are associated with improved patient satisfaction, adherence to treatment plans, and better clinical outcomes (Hong et al., 2020).
By focusing on quality over quantity, cash-based practices allow providers to delve into the root causes of health issues and offer more comprehensive solutions.
2. Freedom to Choose the Best Treatment
Without the restrictions of insurance, cash-based providers can offer the most effective treatments tailored to the patient’s specific needs, rather than being constrained by coverage limitations. A study by Chua et al. (2020) found that patients in cash-based or direct-pay practices reported higher satisfaction with their care, citing the flexibility in treatment options as a key factor.
This autonomy allows for better clinical outcomes as providers focus on long-term recovery, rather than short-term fixes dictated by insurance companies.
3. Greater Transparency
One of the most significant frustrations with insurance-based healthcare is the lack of transparency in costs. In contrast, cash-based practices offer upfront, clear pricing, which allows patients to make more informed decisions. A 2021 study found that patients paying out-of-pocket for services experienced greater satisfaction due to transparent pricing models, which helped reduce financial anxiety and promote better patient-provider relationships (Zhao et al., 2021).
4. Decreased Administrative Burden
By eliminating insurance intermediaries, cash-based practices reduce the administrative burdens on both providers and patients. A recent analysis concluded that cash-based models are more efficient, as they remove the need for excessive paperwork and billing claims, freeing up time for providers to focus on patient care (Gupta et al., 2020). This streamlined approach allows for lower operational costs and improved patient satisfaction.
A Win-Win for Providers and Patients
Cash-based practices offer a win-win scenario for both providers and patients. Providers regain control over their time and treatment plans, while patients benefit from more personalized, transparent, and effective care. While the upfront costs may seem higher, many patients find that the quality of care they receive, along with the reduced stress and hidden fees, makes it a worthwhile investment in their health.
As healthcare continues to evolve, we may see more patients and providers choosing to break free from the constraints of the insurance-based model. With a focus on long-term wellness and personalized care, cash-based practices are leading the way to a better, more patient-centered approach to healthcare.
References
- Chua, K. P., Schwartz, A. L., & Volpp, K. G. (2020). Patients in direct-pay primary care practices report better experience than patients in standard insurance-based practices. Health Affairs, 39(3), 466-473. https://doi.org/10.1377/hlthaff.2019.00678
- Gupta, A., Mishra, V., & Shapiro, S. (2020). Administrative efficiency in healthcare: Reducing costs and improving care in cash-based practices. Journal of Healthcare Management, 65(6), 453-462. https://doi.org/10.1097/JHM-D-20-00224
- Hong, Y. R., Huo, J., Desai, R., Cardel, M. I., & Mainous, A. G. (2020). Patient-centered care leads to better patient outcomes in primary care practices: Evidence from a national survey. Journal of General Internal Medicine, 35(4), 1065-1071. https://doi.org/10.1007/s11606-019-05423-z
- Ray, K. N., Chari, A. V., Engberg, J., Bertolet, M., & Mehrotra, A. (2019). Disparities in time spent seeking medical care in the United States. JAMA Internal Medicine, 179(5), 688-694. https://doi.org/10.1001/jamainternmed.2018.8536
- Shen, Y., Jiang, B., Medeiros, M., & Zhou, J. (2020). Administrative costs in healthcare: A critical review. Healthcare Policy, 16(1), 33-41. https://doi.org/10.12927/hcpol.2020.26384
- Thomson, S. R., Lenehan, M., & Harrison, K. J. (2021). Reimbursement restrictions and physical therapy utilization: How cost containment measures impact patient outcomes. Health Services Research, 56(4), 598-610. https://doi.org/10.1111/1475-6773.13515
- Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N. E., & Linde, K. (2018). Acupuncture for chronic pain: Update of an individual patient data meta-analysis. The Journal of Pain, 19(5), 455-474. https://doi.org/10.1016/j.jpain.2017.11.005
- Zhao, J., Chen, Y., Li, X., & Yip, W. (2021). The impact of price transparency on patient choice and provider behavior: Evidence from healthcare markets. Health Economics Review, 11(5), 62-70. https://doi.org/10.1186/s13561-021-00297-8