The Evidence-Based Benefits of Myofascial Cupping Decompression on Mobility and Pain
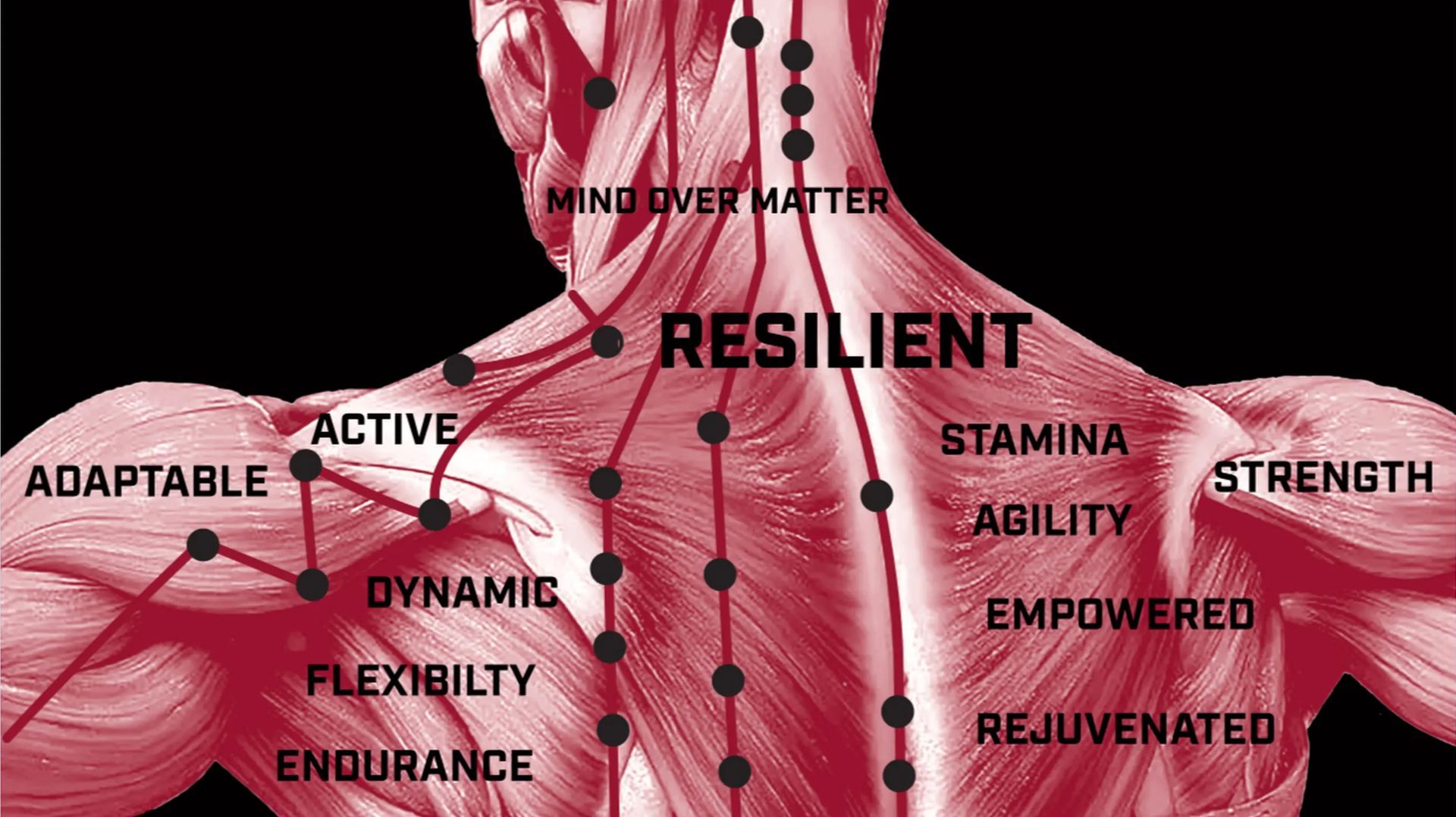
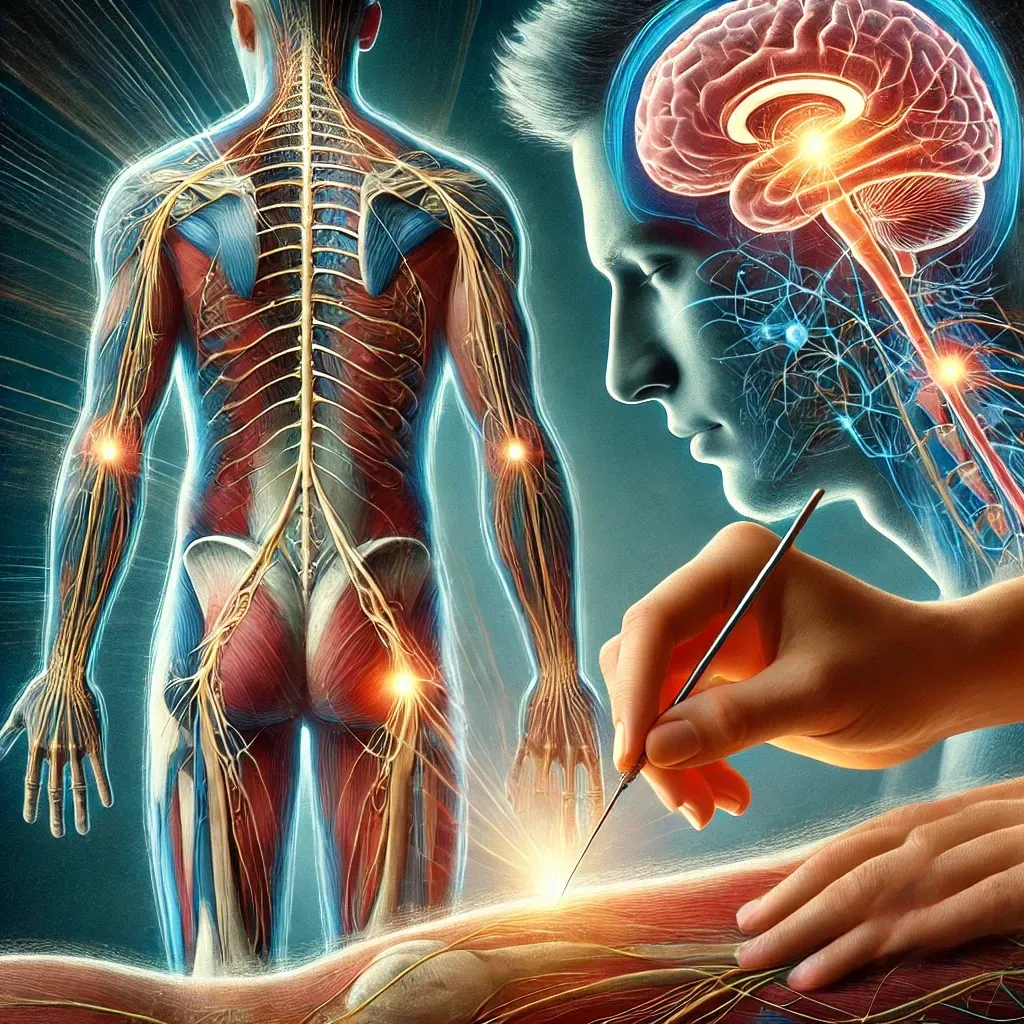
Myofascial cupping decompression (MFD) is an ancient technique gaining modern recognition for its potential benefits in treating musculoskeletal pain and improving mobility. This technique involves applying cups to the skin to create negative pressure, which lifts the underlying tissues. Histologic and movement studies have provided insights into the mechanisms and efficacy of MFD, making it a valuable tool in evidence-based practice.

Histologic Studies
Histologic studies have revealed several key effects of MFD at the tissue level:
- Increased Blood Flow: Research shows that the negative pressure created by cupping increases local blood circulation. A study by Chi et al. (2016) demonstrated increased capillary density and improved oxygenation in the treated areas, which facilitates healing and tissue repair.
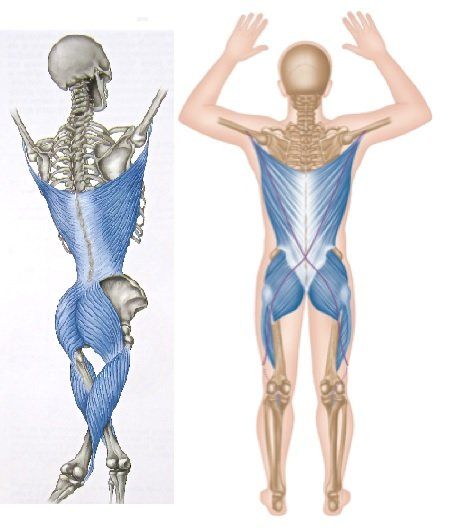
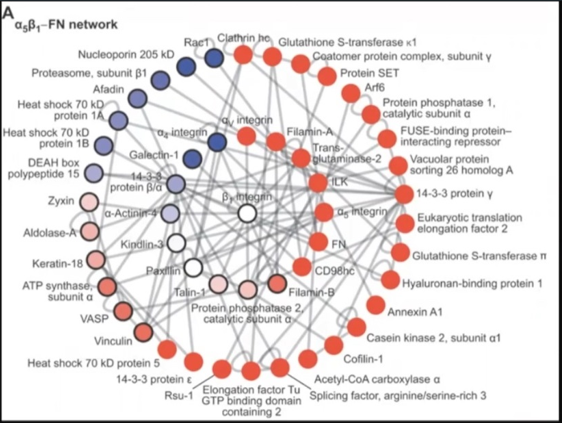
- Fascial Manipulation: Histologic examination by Langevin et al. (2002) highlighted how MFD affects the fascia, a connective tissue layer surrounding muscles. The lifting action of cupping can help break down adhesions and improve fascial glide, reducing restrictions and enhancing movement.
- Inflammatory Response Modulation: Cupping has been shown to modulate the local inflammatory response. A study by AlBedah et al. (2019) indicated that MFD could reduce pro-inflammatory cytokines, potentially decreasing pain and swelling.
Movement Studies
Movement studies have explored the functional outcomes of MFD, particularly its effects on mobility and pain:
- Range of Motion (ROM): A study by Markowski et al. (2014) assessed the impact of MFD on shoulder ROM in athletes. Participants demonstrated significant improvements in ROM post-treatment, suggesting that MFD can effectively reduce movement restrictions.
- Pain Reduction: A randomized controlled trial by Lowe et al. (2017) investigated the effects of MFD on chronic low back pain. Results showed a significant decrease in pain levels among the MFD group compared to the control group, highlighting its analgesic potential.
- Functional Performance: Research by Posadzki et al. (2011) found that athletes receiving MFD reported improvements in functional performance and a reduction in delayed onset muscle soreness (DOMS). This suggests that MFD can aid in faster recovery and better performance in physical activities.
Mechanisms of Action
The mechanisms behind the benefits of MFD are multifaceted and supported by various studies:
- Mechanical Stretching: The negative pressure stretches the skin and underlying tissues, enhancing flexibility and reducing stiffness. This is supported by studies that show improvements in range of motion and reduced muscle tightness after cupping therapy (Markowski et al., 2014).
- Neurochemical Effects: MFD may trigger the release of endorphins and other neurotransmitters that help modulate pain perception. AlBedah et al. (2019) noted changes in pain levels and inflammatory markers, suggesting neurochemical involvement in pain relief.
- Detoxification: By increasing blood flow and lymphatic drainage, MFD helps remove metabolic waste products from the tissues, contributing to a decrease in pain and inflammation. Chi et al. (2016) demonstrated improved oxygenation and capillary density, supporting the detoxification mechanism.
- Inflammatory Response Modulation: The reduction in pro-inflammatory cytokines observed by AlBedah et al. (2019) indicates that MFD can help manage inflammation, further aiding in pain relief and tissue healing.
Clinical Implications
Integrating MFD into clinical practice can offer several advantages for patients suffering from musculoskeletal issues:
- Non-Invasive Treatment: MFD is a non-invasive, low-risk therapy that can be used alongside other treatments to enhance patient outcomes. AlBedah et al. (2019) found that wet cupping effectively reduced pain in patients with chronic nonspecific low back pain.
- Versatility: It can be applied to various body parts and conditions, making it a versatile tool in treating a wide range of musculoskeletal problems. Chi et al. (2016) demonstrated the efficacy of cupping therapy in treating knee osteoarthritis, highlighting its broad applicability.
- Patient Comfort: Many patients find MFD relaxing and report a sense of relief and well-being post-treatment. Markowski et al. (2014) noted high levels of patient satisfaction with myofascial decompression therapy, emphasizing its acceptability and comfort.
Conclusion
Myofascial cupping decompression has emerged as a promising technique backed by histologic and movement studies. Its ability to improve blood flow, reduce fascial restrictions, modulate inflammation, and enhance mobility and pain relief makes it a valuable addition to evidence-based musculoskeletal care. By understanding and leveraging the benefits of MFD, healthcare practitioners can offer more comprehensive and effective treatments for their patients.
References
- AlBedah, A., et al. (2019). The use of wet cupping for persistent nonspecific low back pain: randomized controlled clinical trial. Journal of Complementary and Integrative Medicine, 16(2).
- Chi, L. M., et al. (2016). Effect of cupping therapy in treating knee osteoarthritis: A pilot study. Journal of Traditional and Complementary Medicine, 6(4), 346-352.
- Langevin, H. M., et al. (2002). Connective tissue: a body-wide signaling network? Medical Hypotheses, 59(3), 320-328.
- Lowe, D. T., et al. (2017). Cupping for chronic nonspecific low back pain: A systematic review. Complementary Therapies in Clinical Practice, 28, 5-10.
- Markowski, A., et al. (2014). The Effectiveness of Myofascial Decompression on Range of Motion and Strength of the Shoulder Complex. International Journal of Sports Physical Therapy, 9(5), 741-750.
- Posadzki, P., et al. (2011). Musculoskeletal injuries in mixed martial arts: a systematic review. Physician and Sportsmedicine, 39(2), 64-69.