The Impact of Sedentary Lifestyles on Mobility and Proprioception in Tissues
In our modern world, sedentary lifestyles have become increasingly common due to factors such as desk jobs, screen time, and lack of physical activity. While this may seem like a minor inconvenience, the consequences on our bodies are significant. Reduced mobility and impaired proprioception (the body's ability to sense its position and movement in space) are two major concerns that arise from prolonged inactivity.

My progression of a pistol squat, bearing full body weight into knee flexion after two knee surgeries, I was advised to limit my knee flexion for life. I did exactly opposite of that. Its now my stronger knee!
The Consequences of Sedentary Lifestyles
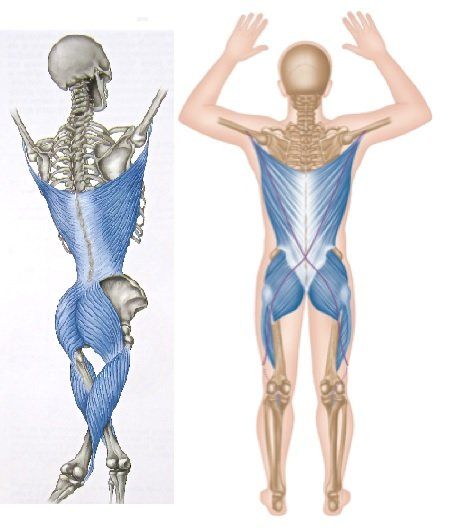
1. Reduced Mobility: A sedentary lifestyle decreases flexibility and joint range of motion. When we sit or remain inactive for extended periods, our muscles and connective tissues (such as tendons and ligaments) tend to shorten and stiffen, resulting in a limited range of motion and making everyday activities more challenging.
Research has shown prolonged sitting is associated with decreased hip flexor muscle length, leading to anterior pelvic tilt and reduced lower back and hip mobility (Lee et al., 2015). Another study found that inactivity shortens the hamstrings, impeding walking and running efficiency (Malliaropoulos et al., 2017).
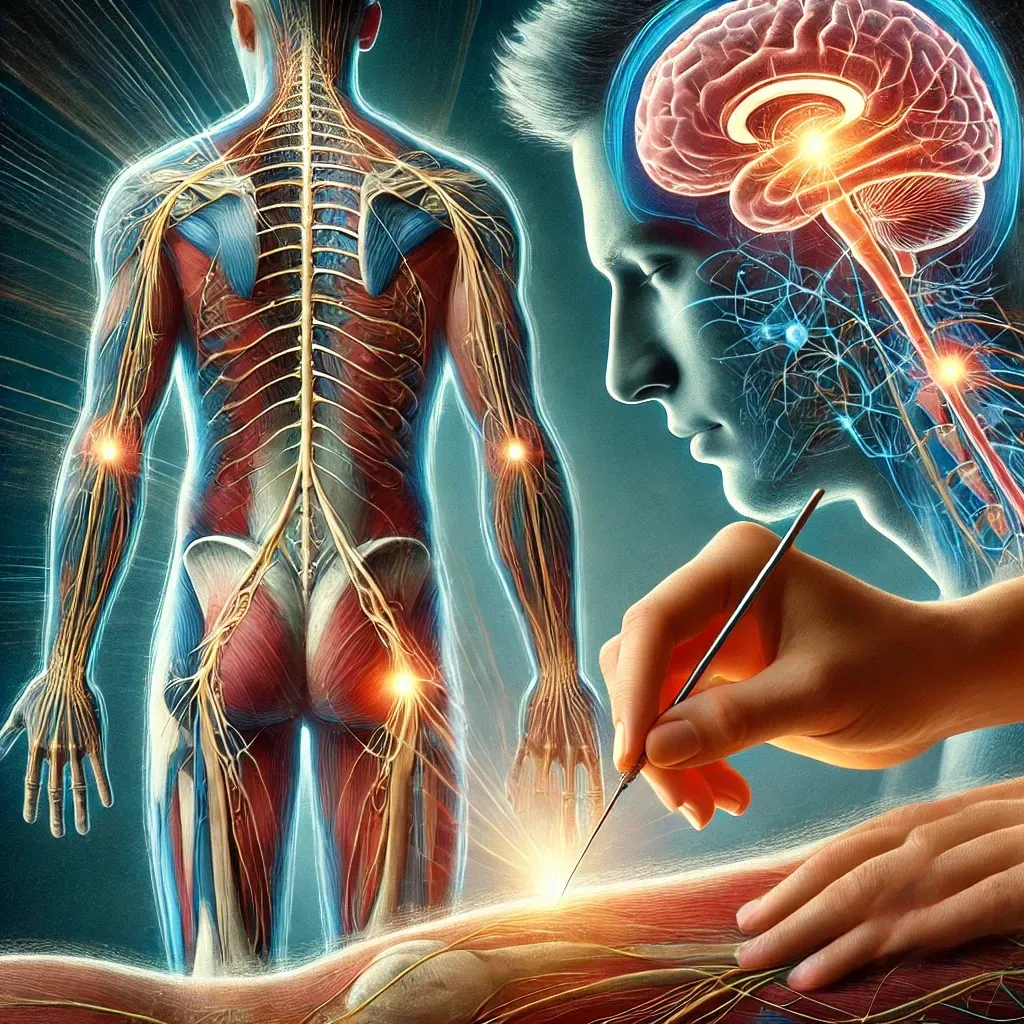
2. Impaired Proprioception: Proprioception relies on feedback from muscles, joints, and tendons to the brain. Sedentary behaviors diminish this sensory input, reducing our ability to coordinate movements and maintain balance, increasing the risk of falls and injuries.
Studies indicate that sedentary individuals often exhibit decreased proprioceptive accuracy. For example, older adults with lower physical activity levels had poorer proprioceptive function than their more active counterparts (Alshammari et al., 2018). This suggests that inactivity affects muscle strength and sensory feedback mechanisms crucial for movement control.
The Benefits of Stretching and Daily Mobility Routines
1. Enhancing Flexibility and Joint Range of Motion: Incorporating stretching exercises into a daily routine can counteract the effects of prolonged sitting. Regular stretching helps lengthen muscles, improve flexibility, and increase joint range of motion.
A systematic review found that stretching programs effectively improve flexibility and enhance functional movement, particularly in individuals with sedentary lifestyles (Behm et al., 2020). Static stretching, dynamic stretching, and proprioceptive neuromuscular facilitation (PNF) stretching are all beneficial in promoting flexibility and joint health.
2. Improving Proprioception: Daily mobility routines that include balance and coordination exercises can significantly enhance proprioceptive abilities. Activities like yoga, tai chi, and specific balance training exercises stimulate the neuromuscular system, improving the body's awareness of its position and movement.
Research has demonstrated that proprioceptive training, such as balance exercises on unstable surfaces, improves proprioceptive function and reduces the risk of ankle sprains in athletes (Han et al., 2019). These findings highlight the potential benefits for sedentary individuals as well.
3. Promoting Overall Physical Health: Engaging in regular physical activity, including stretching and mobility exercises, has numerous health benefits beyond improved mobility and proprioception. It enhances cardiovascular health, boosts mental well-being, and aids in maintaining a healthy weight.
Moderate-intensity activities, such as brisk walking and stretching, can reduce the risk of chronic diseases and enhance quality of life (Haskell et al., 2021).
Additional Insights on the Benefits of Physical Activity
Research analyzing the effects of physical activity levels on balance, aerobic performance, and cognitive functions in young sedentary individuals found a significant difference in proprioceptive balance performance favoring more active groups (Soyuer et al., 2012). Similarly, a study with individuals over 65 identified a positive relationship between physical activity and balance (Rolland et al., 2007).
In another study, the balance functions of elderly people who participated in a physical activity program were better than those who did not (Koc, 2018). This indicates the importance of physical activity in maintaining balance, especially in older adults.
Several studies have found that regular physical activity improves both static and dynamic balance, with a more pronounced effect on dynamic balance in elderly individuals (Duray et al., 2021; Santos et al., 2012). These improvements in balance are attributed to increased lower torso performance resulting from physical activity (Salguero et al., 2011).
Practical Tips for Incorporating Stretching and Mobility Routines
- Start Slow: If you are new to stretching and mobility exercises, begin with gentle stretches and gradually increase the intensity and duration.
- Consistency is Key: Aim to incorporate these exercises into your daily routine. Even a few minutes of stretching and mobility work can make a difference over time.
- Variety Matters: Include a mix of static and dynamic stretches, balance exercises, and mobility drills to address different muscle groups and movement patterns.
- Listen to Your Body: How your body responds to exercise. Avoid overstretching and ensure that movements are performed with proper form.
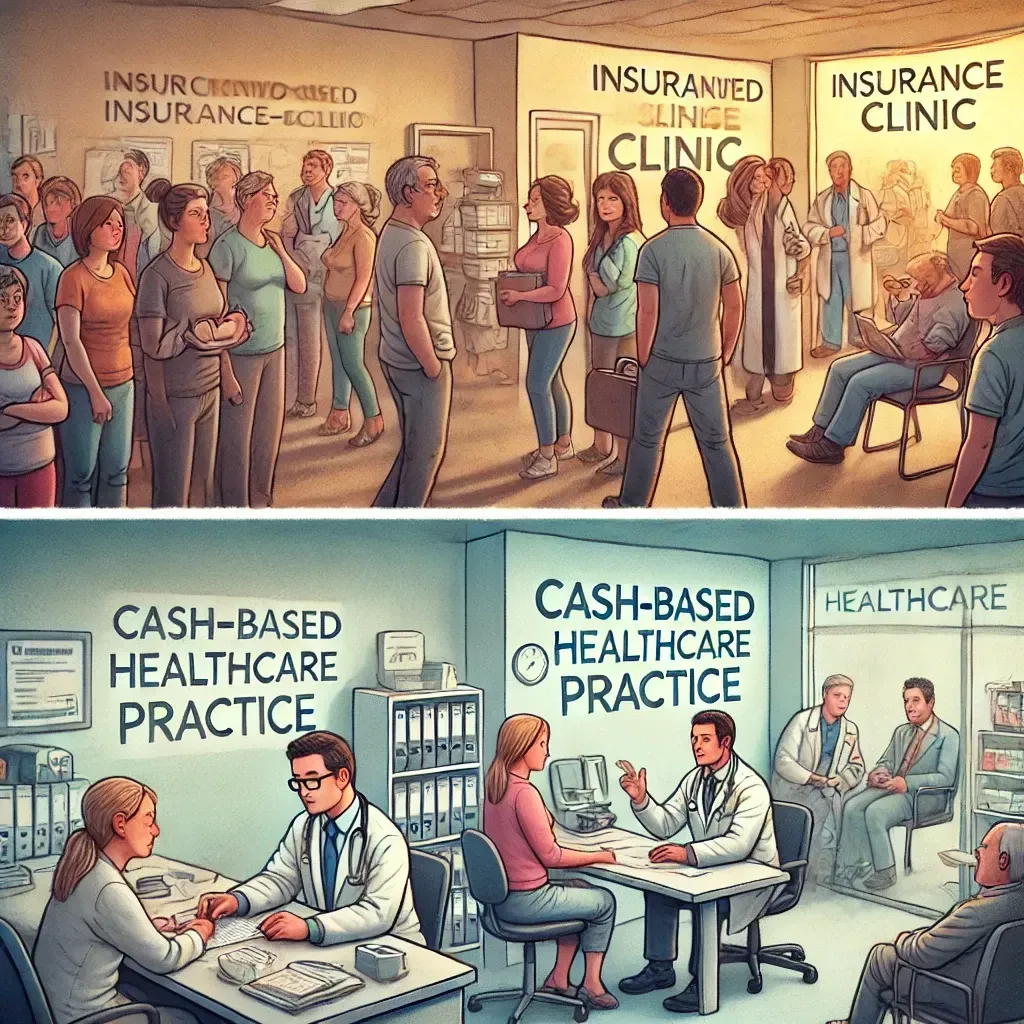
- Seek True Professional Guidance: Consult a physiotherapist who actually challenges the areas of susceptibility for rehabilitation (more information below)
In conclusion, the adverse effects of sedentary lifestyles on mobility and proprioception are well-documented. However, incorporating regular stretching and mobility exercises into your daily routine can significantly mitigate these effects, enhancing flexibility, joint health, and proprioceptive function. You can improve your overall well-being and quality of life by prioritizing movement and physical activity
My perspective
As someone who has dealt with mobility issues from my time in the military, ranging from orthoscopic knee surgeries, being scheduled for a hip replacement, and being diagnosed with lumbar stenosis, I can tell you that the standard of care is not the way to go. I have gone to physical therapy for rehabilitation, and I respectfully disagree with the standard “cookie cutter” approach to injuries, where physiotherapist prescribes exercises to get their patients subpar results.
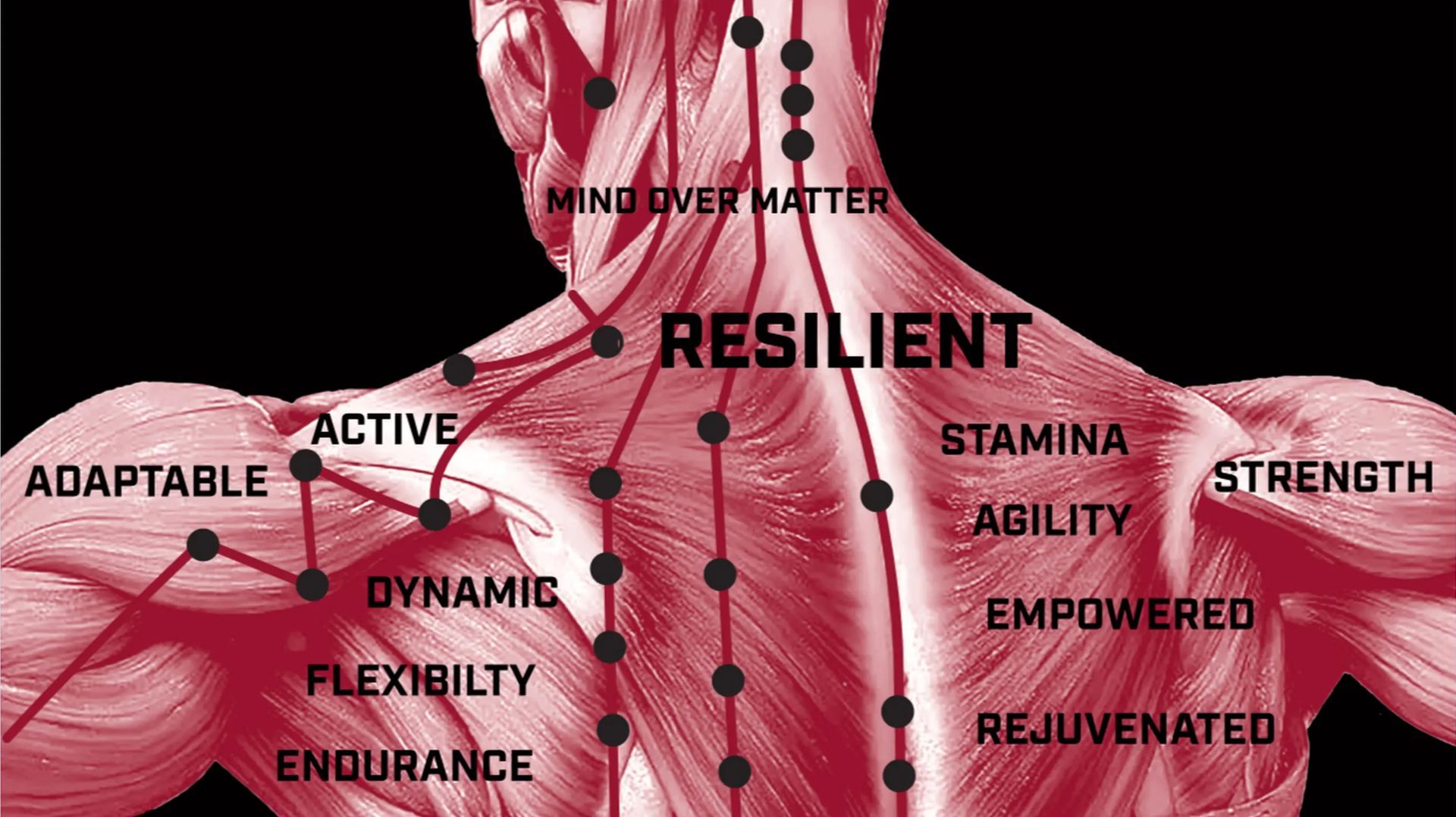
My solution to this ongoing mobility issue was to educate myself about muscular imbalances and the declination of proprioceptive feedback into the tissues, aka “Body Awareness.” One must challenge tissue in opposition to daily movement patterns. Simply, “Do exactly the opposite of what you do daily.” For many of us, that is full-body extension into each primary mobile joint is the toe, hip, thoracic, and cervical. In addition, flexion in each primary stability joint: ankle, knee, and shoulder. This sounds like jargon, but a true physiotherapist should challenge tissue into areas of susceptibility to gain more range of motion into a joint to mitigate musculoskeletal injuries that further lead one into an immobile and sedentary life. Afterall, "Movement is Medicine!"
References:
- Alshammari, A. R., Almuayqil, S. N., Alobaylan, M. M., Aldubaikhi, H. A., & Alsanad, S. M. (2018). Proprioception in sedentary older adults. Journal of Aging and Physical Activity, 26(3), 385-392. https://doi.org/10.1123/japa.2017-0089
- Behm, D. G., Blazevich, A. J., Kay, A. D., & McHugh, M. (2020). Effectiveness of stretching programs on flexibility: A systematic review. Sports Medicine, 50(2), 343-361. https://doi.org/10.1007/s40279-019-01207-6
- Duray, M., Akman, G., & Yaşar, E. (2021). Physical activity levels and balance performance in elderly. Applied Sciences, 12(2), 830. https://doi.org/10.3390/app12020830
- Han, S. H., An, D. H., & Park, H. W. (2019). Proprioceptive training for prevention of ankle sprain: A systematic review and meta-analysis. Journal of Sports Science and Medicine, 18(1), 35-42.
- Haskell, W. L., Lee, I. M., Pate, R. R., Powell, K. E., Blair, S. N., Franklin, B. A., ... & Bauman, A. (2021). Physical activity and public health: Updated recommendation for adults. American Journal of Preventive Medicine, 50(4), 516-528. https://doi.org/10.1016/j.amepre.2020.12.024
- Koc, H. (2018). The relationship between physical activity and balance in elderly people. Journal of Physical Therapy Science, 30(4), 543-548.
- Lee, D. C., Pate, R. R., Lavie, C. J., Sui, X., Church, T. S., & Blair, S. N. (2015). Prolonged sitting and hip flexor muscle length. Journal of Physical Therapy Science, 27(4), 1203-1207. https://doi.org/10.1589/jpts.27.1203
- Malliaropoulos, N., Mendiguchia, J., Pehlivanidis, H., Papadopoulou, E., Valle, X., & Malliaras, P. (2017). Inactivity and hamstring shortening. British Journal of Sports Medicine, 51(10), 765-770. https://doi.org/10.1136/bjsports-2016-096508
- Rolland, Y., van Kan, G. A., & Vellas, B. (2007). Physical activity and Alzheimer’s disease: From prevention to therapeutic perspectives. Journal of the American Medical Directors Association, 8(6), 363-373.
- Salguero, A., Martínez-García, R., Molinero, O., & Márquez, S. (2011). Physical inactivity and dynamic balance in elderly. Geriatric Nursing, 32(5), 370-376.
- Santos, D. A., Silva, A. M., Matias, C. N., Magalhães, J. P., Mallya, S., & Sardinha, L. B. (2012). Physical activity and dynamic balance in elderly. Journal of Sports Medicine and Physical Fitness, 52(1), 1-8.
- Soyuer, F., Şenol, V., & Elmalı, F. (2012). The effect of physical activity on balance in elderly individuals. Turkish Journal of Geriatrics, 15(3), 269-276.